






























.jpeg)

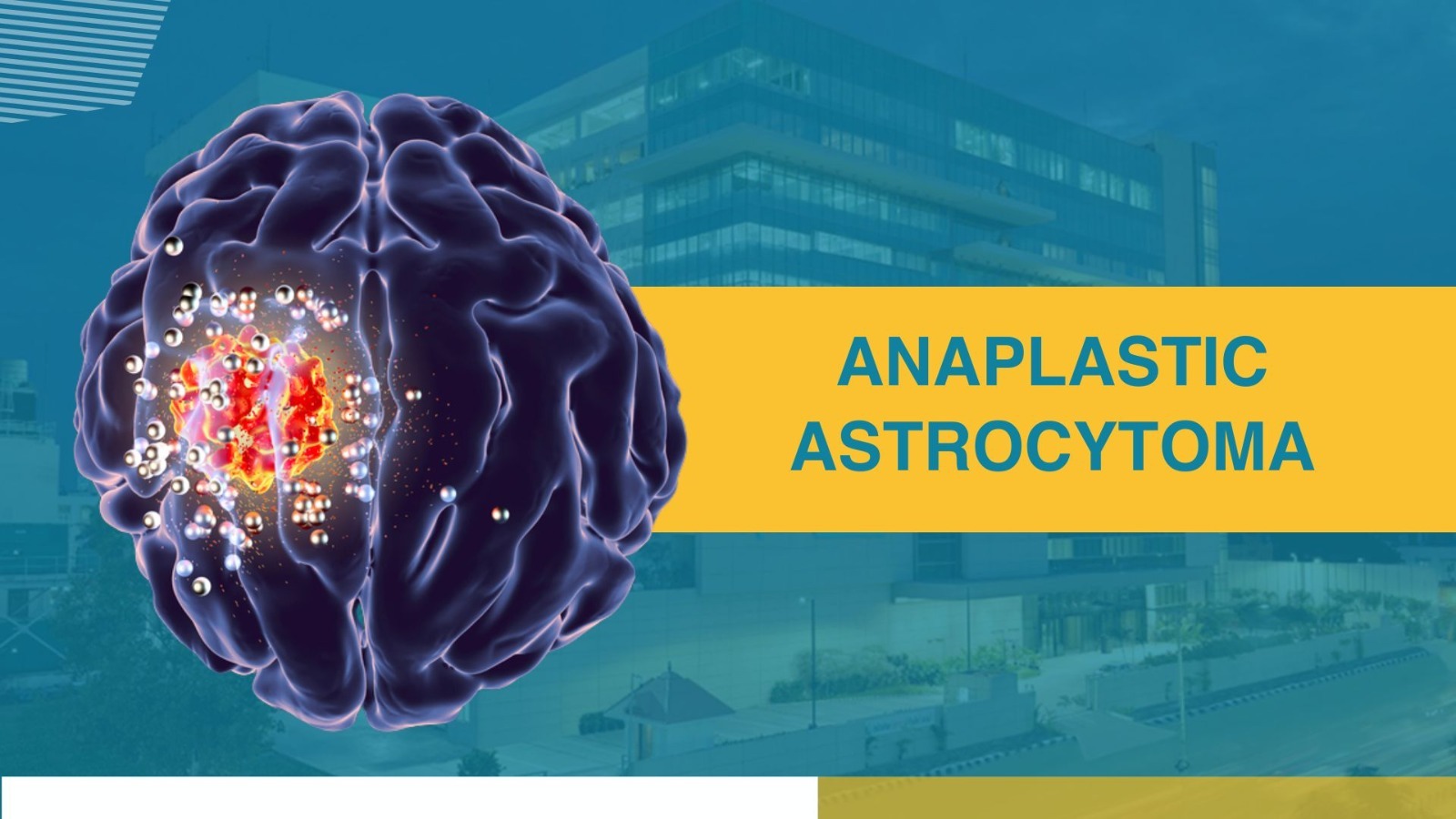
Winning over Cancer with Apollo Proton Cancer Centre
A breakthrough in Cancer Care! The global growing cancer burden tells an ominous tale. To counter this growing threat, Apollo Proton Cancer Centre provides a complete and comprehensive solution. As cancer care has become one of the fastest-growing healthcare imperatives across the world, we believe it is critical to redefine our purpose, to reboot our commitment on the single-minded focus - to battle cancer, to conquer cancer! APCC stands as a ray of hope for millions, infusing them with the courage to stand and stare cancer down.

Copyright © 2023 Apollo Proton Cancer Centre. All Rights Reserved





