Every time we perform a skull base surgery, we get fresh knowledge into addressing the existing pathology. This article will discuss how endoscopic methods have made the essential procedure less difficult.
Skull base surgery has long been a litmus test for talent and competence. Important blood arteries and cranial nerves pass via several foramina in the skull base, complicating the surgery. Over the years, particularly in the last decade, there has been a significant revolution in skull base operations, with a shift from microscopic to endoscopic techniques.
Endoscopic endonasal surgery allows access to nearly every section of the skull base, from the Crista galli to the foramen magnum. The majority of diseases involving these regions are tumors, however CSF rhinnorhea, other chronic infections such as mucormycosis (fungal), congenital deformities such as encephalocoele, traumatic optic canal fractures, fibrous dysplasia, and other conditions can also occur.
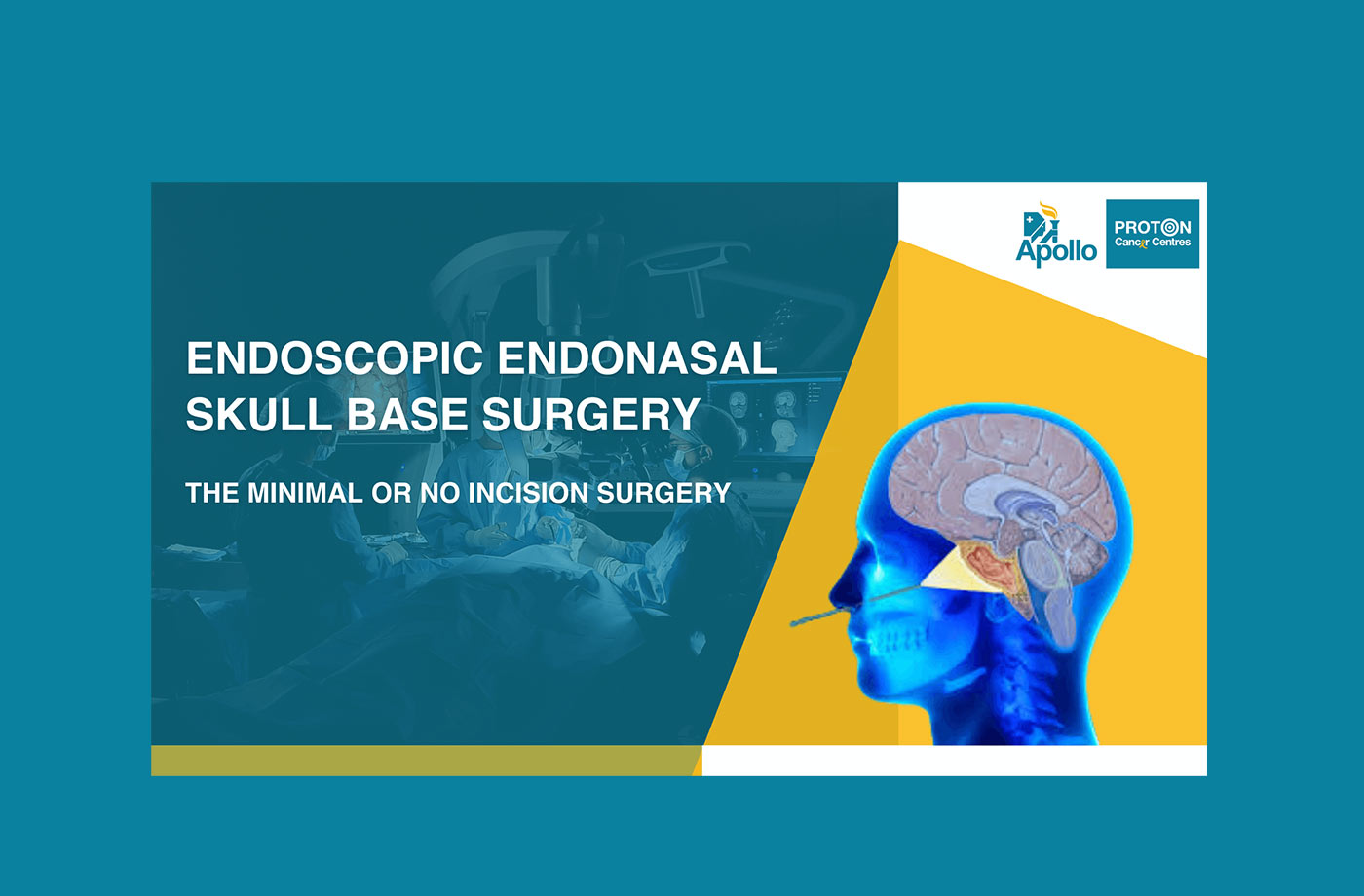
Endonasal endoscopic resections have the benefit of allowing us to access the tumor with minimum or no incision over the head. Many tumors in the skull base are placed in crucial areas, such as in and around the optic nerves, carotid arteries, and cranial nerves. It is critical to remove the lesions that are pushing on the cranial nerves.
Simple endoscopic skull base resection to prolonged Endoscopic Endonasal techniques can be performed in this area. There are several adjuncts available to aid with Endoscopic Endonasal surgery. Depending on the amount of resection, both uni-nostril and bi-nostril procedures can be performed. It is always preferable to have an ENT surgeon and a skull base surgeon work together to get the best resection and repair in Endoscopic Endonasal Sinus procedures.
Endoscopic surgery has made enormous advances, such as navigation, curved drills for skull base drill, curved suction tips, and bone removal cusa, which have increased the safety of skull base procedures. When it comes to skull base procedures, reconstruction is crucial since the most feared early consequence is a postoperative CSF leak. The introduction of Pedicle Nasoseptal flaps as well as other safety measures has reduced problems to a larger extent.
Not only do we employ angiography, but we also use ICG-enabled surgery to detect and find the internal carotid artery during skull base dissection. Intraoperative CT and MRI scans provide an added benefit to the complete resection.
Recent research suggests that reducing volume from tumors placed near essential radiation-sensitive tissues is a good surgical objective to prevent possible harm and negative impacts during radiation therapy.
To reduce the chance of a spinal fluid leak, patients are encouraged to limit actions that might raise the pressure of spinal fluid within the head (bending, straining, lifting, nose-blowing) for a month after surgery.
They are also recommended to come in on a regular basis for an endoscopic evaluation of the nasal cavity and the removal of nasal crusts. Healing is complete, and crusting normally fades after 3 to 4 months. Their extra follow-up is tailored to the pathological result of the lesion, the necessity for additional therapy, and the severity of their symptoms.
Due to restricted air flow through the nose, some patients may have modest loss of smell and taste for several months after surgery. This can be reduced by avoiding excessive cautery use in and around the cribriform plate of the ethmoid and the Crista galli area.
Endoscopic surgery improves accuracy and precision while causing relatively little stress. Our Centre has seen greater results with a lot simpler and more pleasant technique. Patients heal faster and stay in the hospital for a shorter period of time. In contrast to standard craniotomies, there is minimal stress to the structures of the face and skull, as well as modest aesthetic influence.

Copyright © 2023 Apollo Proton Cancer Centre. All Rights Reserved