Cell types
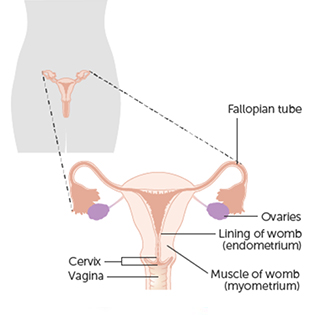
The cervix is covered with a layer of skin-like cells on its outer surface, called the ectocervix. Inside of the cervix, there are glandular cells that produce mucus. This is called the endocervix.
The skin-like cells of the ectocervix can become cancerous, leading to squamous cell cervical cancer. This is the most common type of cervical cancer.
The glandular cells of the endocervix can also become cancerous, leading to adenocarcinoma of the cervix.
Transformation zone
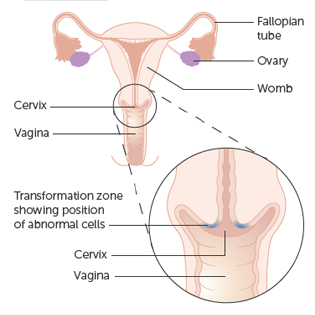
The area where cervical cells are most likely to become cancerous is called the transformation zone. It is the area just around the opening of the cervix that leads on to the endocervical canal.
The endocervical canal is the narrow passageway that runs up from the cervix into the womb.
Cervical screening
The transformation zone is the area that your doctor or nurse checks during cervical screening.
Cervical screening is not a test for cancer. It is a test to pick up abnormal cervical cells. If left untreated, the abnormal cells might develop into cancer.
Lymph nodes
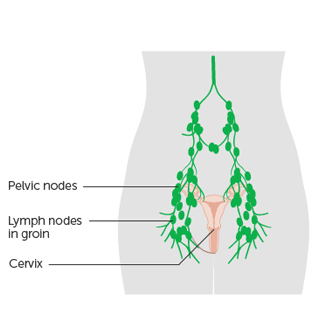
Like all other areas of the body, there are lymph nodes around the womb and cervix. The nearest large group of lymph nodes are at the top of the leg (the groin area).
Lymph nodes (also called lymph glands) are part of the lymphatic system. They:
- help to protect the body against infections
- filter, drain and circulate the tissue fluid that bathes all body cells and tissues
Lymph nodes are also important in cancer. The tissue fluid that bathes the area containing the cancer, drains to the nearest lymph nodes. So if any cancer cells break away from the tumour, the first place they can go is to the nearest lymph nodes.
When you have surgery for cervical cancer, your surgeon usually takes out some lymph nodes. They send them to the laboratory to check for cancer cells.