Most women will have surgery for womb cancer. Find out about surgery, including what to expect before and after your operation.
Minimally invasive (Laparoscopic/ Robotic) Hysterectomy for Endometrial Cancer
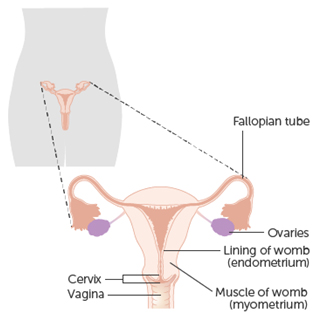
Women with cancer of the lining of the womb (uterus) need an operation to remove their womb, fallopian tubes and ovaries. This operation may be carried out using key-hole surgery.
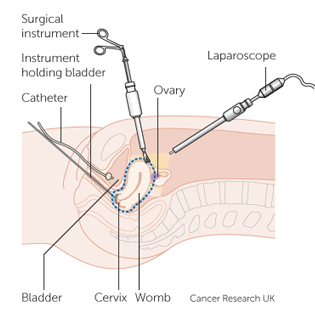
There are two minimally invasive approaches: laparoscopic and robotic-assisted surgery, possibly with da Vinci technology. Surgeons perform minimally invasive laparoscopic or robotic-assisted surgeries through a few small incisions. In laparoscopic surgery, surgeons use special long-handled tools while viewing magnified images from the laparoscope (camera) on a video screen.
Surgeons can perform Robotic hysterectomies for cancer using da Vinci technology. With da Vinci, your surgeon sits at a console next to you and operates using tiny, fully wristed instruments.
A camera provides a high-definition, 3D magnified view inside your body. Every hand movement your surgeon makes is translated by the da Vinci system in real-time to bend and rotate the instruments with precision.
Compared to patients who had an open procedure, patients who had a hysterectomy with da Vinci experienced fewer complications and stayed in the hospital for less time. Compared to patients who had a laparoscopic procedure, patients who had a hysterectomy with da Vinci had fewer, or similar, complications and stayed in the hospital for the same, or less, time.
The womb (uterus) along with the cervix (neck of the womb), fallopian tubes and ovaries are removed (bilateral salpingo-oophorectomy). Sometimes it is necessary to remove some lymph nodes in the pelvis. Your surgeon will discuss this with you before your operation.
The operation aims to remove all of cancer. If there is any evidence that cancer has spread, or if the results of the operation suggest that you may be at increased risk of recurrence of cancer (your cancer returning), you may be offered further treatment such as radiotherapy and/ or chemotherapy. This will be discussed with you when all of your results are available.
If there is an advanced disease (cancer spread to other organs) at the time of having a look with the telescope your surgeon may abandon the procedure and you have chemotherapy upfront and have surgery at a later date or the surgeon might perform an operation removes all cancer(debulking) either by minimally invasive procedure or by giving a cut (laparotomy).
Having an MIS instead of through a large cut on your abdomen (tummy) should result in a shorter hospital stay, less scarring on your tummy and a quicker recovery.
The advantages of using a robot or laparoscope include Shorter hospital stay, less pain, less risk of wound infection, less blood loss reducing the need for a blood transfusion, less scarring, faster recovery, quicker return to normal activities such as driving.