- Chest X-rays look for a mass or spot on the lungs.
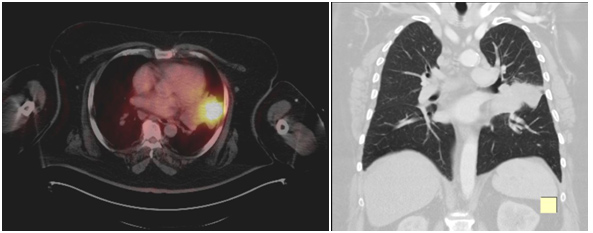
- Imaging tests, such as CT scan, PET scan, bone scan, MRI and ultrasound that show detailed images of the lungs and other parts of the body.
- Bronchoscopy guided interventions also help in diagnosing these cancers.
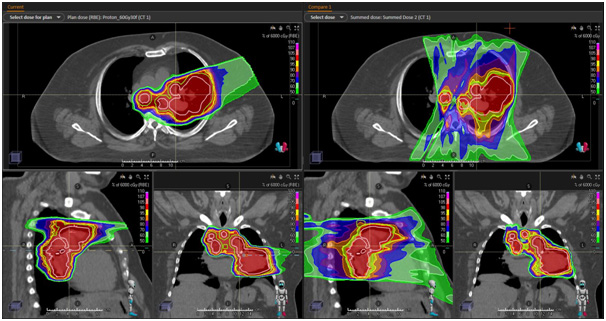
Mr. Praboth Palit from Mumbai shares an emotional journey of his treatment at Apollo
Proton Cancer Centre. Despite facing a lot of challenges in the beginning, Praboth never
lost his hope which is highly commendable.
He thanked Mr. John Chandy , Dr.
Srinivas Chilukuri, and the entire team for their support and guidance.