When is Radiation therapy advised in prostate cancer?
Radiation therapy for prostate cancer is one of the most common treatment treatments offered for Prostate Cancer. It has a potential role in almost every stage of prostate cancer-from early stage to an advanced stage.
- Radiation therapy can be offered in the early stages of prostate cancer as a single curative modality. Large randomized clinical trials have shown that the long term results of radiation therapy are equivalent to surgery in this early-stage prostate cancer. Radiation therapy has been shown to yield a nearly 95% survival rate in this stage.
- Radiation therapy can be offered in high-risk or locally advanced cancers along with hormone therapy also called androgen deprivation therapy. In this stage also, radiation and androgen deprivation therapy can yield a long-term survival of 80-90%.
- Radiation therapy can be given as a postoperative treatment after radical prostatectomy either due to residual disease after surgery or due to an increase in serum prostate-specific antigen after surgery. If done at the appropriate time, the likelihood of long-term cure in this subset is also around 80%.
- Radiation therapy can be offered as a curative treatment along with hormone therapy as well as newer drugs in advanced or metastatic prostate cancer if the metastases are limited to a few sites or a few lymph nodes. This stage of the disease is called oligometastatic disease as the metastatic burden is limited.
- Radiation therapy can be offered as a palliative treatment for the palliation of bone pain, bleeding, etc in advanced or metastatic prostate cancer.
Radiation therapy is a non-invasive form of treatment that has shown to yield equivalent results to invasive surgery. The choice of treatment depends on patient symptoms, preference and logistics.
What is the duration of treatment?
Duration of prostate cancer treatment varies, ranging from 7-8 weeks for conventional treatment, to 4 weeks with hypofractionated treatment. Most treatments worldwide have been reduced to 4-5 weeks in patients with intact prostate. Large scale randomized trials have shown that shorter schedules are as efficacious as prolonged schedules and result in similar toxicities thereby improving patient convenience.
Postoperative radiation therapy is usually given for about 6-7 weeks. Also, treatment is exclusive of simulation and planning, which usually takes about a week before the start of treatment.
What are the types of Radiation in prostate cancer?
There are two types of radiation treatment for prostate cancers, which are External beam radiotherapy which includes 3-dimensional conformal radiation therapy, Intensity-modulated radiation therapy, volumetric modulated arc therapy, and Proton beam therapy. All these treatments are delivered with image guidance and hence also referred to as image-guided radiation therapy or IGRT. IGRT in most modern centres involves daily CT imaging.
The other option is brachytherapy, which can be done either via interstitial needle implantation under sedation, which includes placement of needles with template guidance thereby delivering uniform doses to the prostate cancer, and seed implants, which are permanent implants, which are inserted under image guidance and left in the body, which delivers low dose radiation to a prolonged period, thereby treating the malignancy.
Brachytherapy is usually considered for low/intermediate-risk prostate cancers, where the target is mainly the prostatic lesion, whereas external beam radiotherapy is noninvasive and can treat both prostates as well as the involved nodes. Sometimes, a combination of external beam radiotherapy and brachytherapy are also considered based on the clinical decision for high risk localized or locally advanced prostate cancers.
SBRT for prostate cancer
Traditionally, prostate cancers are treated over 7-8 weeks with conventional fractionation. Modern hypofractionation schedules incorporate schedules of treatment for 4-5 weeks. However, Stereotactic body radiotherapy (SBRT) or Stereotactic ablative radiotherapy (SABR) for prostate cancer is a radiation technique where the entire treatment is condensed over five sittings of radiation. It delivers a high dose per fraction, which takes into advantage the radiobiology of prostate cancers. This advantage translates to delivering biologically higher doses of radiation in a shorter period of time without increasing the likelihood of toxicities or side-effects associated with treatment.
In early localized prostate cancers (low and intermediate-risk prostate cancers), SBRT is now considered standard with equivalent cancer control outcomes and limited toxicities. Its role is emerging even in patients with locally advanced and node-positive prostate cancers. The cancer outcomes of SBRT remains the same as that of conventional external beam radiotherapy/brachytherapy or surgery. The biggest advantage is patient convenience which can be completed over a week.
Methods to deliver SBRT
- Linear accelerator-based SBRT
- Dedicate radiosurgery equipment such as Cyberknife
- Proton beam therapy
Radiation for metastatic Prostate Cancer
Radiation therapy can be considered as a curative treatment for metastatic prostate cancers when the metastatic disease burden is limited, i.e, oligometastatic, which means spread of the disease to limited sites or nodes. It can also be considered as a palliative treatment, for control of bone pain, or bleeding, or control of lower urinary tract symptoms, which focus mainly on quality of life for these patients.
Radiation therapy for Prostate cancer - Procedure
Planning typically includes:
Radiation simulation. A few days before your radiation simulation appointment, several marker seeds will be inserted into your prostate by a radiologist. These markers help to locate your prostate more precisely during each radiation treatment session. During the simulation, you must lie down still throughout the procedure. Your radiation therapy team will help you find a comfortable position during treatment. Customized immobilization devices are used to help you hold still in the right position. Your radiation therapy team will make marks on your body to be used during your radiation therapy sessions.
Planning scans. Your radiation therapy team performs computerized tomography (CT) scans to determine the exact area of your body to be treated. After the planning process, your radiation therapy team decides what dose you will receive based on your stage of cancer, your general health and the goals for your treatment.
During a treatment session:
- You lie down in the position determined during your radiation simulation session.
- You might be positioned with customized immobilization devices to hold you in the same position for each therapy session.
- The proton gantry may rotate around your body to deliver radiation beams from different directions.
- You lie still and breathe normally during the treatment.
- Your radiation therapy team stays nearby in a room with video and audio connections so that you can talk to each other.
- You will not feel any pain. Speak up, if you feel uncomfortable.
What can one expect during the treatment?
Generally, side effects do not appear until the second or third week of treatment. As proton therapy is a local treatment, only the areas of the body where it is directed will experience side effects. Most patients will experience some or all of the following:
- Increase in the frequency of urination
- Urinary urgency
- Weak urinary stream
- Difficulty starting urination
- Burning or tingling with urination
- Occasional diarrhea
- Softer and smaller volume bowel movements
- Increased frequency of bowel movements
- Worsening of hemorrhoids or rectal irritation with occasional scant blood and fatigue
Depending on the severity of these side effects, you may be prescribed medications such as anti-diarrheal medication (Immodium or Lomotil) or medication to decrease the frequency of urination (Flomax or Urispas) for symptom relief. Most of these symptoms are short-term and go away after the proton therapy ends. The time for full recovery depends on the patient and the type and severity of urinary or bowel symptoms, and whether the patient had any symptoms before treatment.
As part of your treatment planning, you will be asked to fill out questionnaires to help evaluate your bladder, rectal and sexual function. It is important to discuss the nature and severity of your particular symptoms with your doctor, since this may influence your treatment course. Patients typically continue with their normal daily activities during treatment.
Many questions may arise during radiation therapy treatment. Your doctors will be available to answer questions throughout your treatment.
What are the side effects? What can I do about side effects?
Fatigue — Fatigue may occur later in radiation therapy treatment. Consider taking a nap during the day. If working, consider decreasing work hours or taking leave, if possible. However, try to maintain a level of physical activity and a well-rounded diet. Nutritionists are available to assist if desired. Contact your doctor if fatigue becomes severe. It is typically more in patients who are also receiving concurrent androgen deprivation or hormone therapy.
Diarrhea, flatulence or painful defecation — These symptoms usually occur after the second or third week of treatment. Symptoms will resolve after the treatment ends. During proton therapy, dietary modification usually helps reduce the frequency and severity of diarrhea. Try to avoid or reduce fried foods, greasy foods and highly spiced foods. Reduce foods with insoluble fiber, such as lettuce and cauliflower, and increase low-fiber and soluble-fiber foods, such as bananas, mashed potatoes, applesauce, white rice, canned or cooked fruits and vegetables.
Maintain your intakes of lean proteins, such as pulses, turkey, chicken and fish, and increase your fluid intake to avoid dehydration. Using moist toilet paper, baby wipes or sitz baths may help relieve rectal irritation. Your doctor may recommend anti-diarrheal medications. Contact your doctor if you see blood in your stool, if diarrhea worsens or if you become light-headed or dizzy.
Frequent urination, burning with urination and difficulty urinating — These are the most common complaints. Occasionally the urinary stream will weaken. Generally, these symptoms are managed with medications to help the bladder function better or eliminate burning. Rarely, your doctor may order a urine test. Symptoms will resolve after the end of treatment. Contact your doctor if you see blood in your urine or if you are unable to urinate.
Skin irritation — This is uncommon, but if it occurs, do not rub or scratch the area. Avoid clothing that rubs and avoid alcohol-containing lotions or colognes. Your doctor can recommend a skincare regimen and topical creams or lotions to relieve the symptoms. Contact your doctor if you develop a rash all over your body.
What other special details should I be aware of?
Before you go home, you will be given detailed written instructions about the following issues:
Radiation safety — There is no remaining radiation in your body once your treatment is complete and it is completely safe to be around other people.
Sexual function — A small percentage of men experience a decline in erectile function after radiation therapy. The likelihood of impaired potency is influenced by age, which is the primary risk factor, the use and duration of hormone therapy, smoking and medical conditions, such as hypertension and diabetes, as well as the medications used for their treatment.
The effects of short-term hormone therapy (four to six months) appear to be largely reversible. Similar levels of sexual function are reported at four years by patients who received hormone therapy and patients who did not receive hormone therapy. Most men who are not taking nitrate-containing medications can use any one of the oral medications on the market that improve erectile quality with excellent success. Patients may experience a prolongation of the time to orgasm. Some experience a change like their ejaculates, such as thicker and less fluid, a decrease in the quantity or an absence of ejaculate after radiation treatment. Patients on long-term hormone therapy may have more pronounced sexual dysfunction and you must discuss with your doctor.
Sperm production — Sperm are produced in germinal cells in the testicles. During prostate radiation, low levels of "scatter radiation" that originate inside the patient's body can reach the testicles and decrease sperm production. The dose of radiation that reaches the testicles usually leads to a temporary reduction (months to years) in the sperm count. However, it is possible to have a permanent reduction in sperm count or sterility. If you are considering fathering additional children, you may wish to seek medical advice regarding your fertility and need to bank sperm.
Testosterone production — Testosterone is secreted by the Leydig cells in the testicles. Generally, the doses of internal scatter radiation that reaches the testicles are not high enough to impair Leydig cell function.
Rectal Bleeding — About 2-3% of the patient may have inflammation of the rectum which may result in bleeding. The best way to avoid this side-effect is to avoid constipation. If it is severe and prolonged, you may need an endoscopic intervention or per rectal medications. Please contact your doctor in case that happens.
How often will I need to see my doctor for a follow-up?
Following Proton therapy, you will have an initial appointment to make sure that treatment-related side effects are diminishing or have gone away.
The frequency of follow-up appointments will be based on the risk of cancer recurrence. In general, serial PSA blood tests will start around the third month after treatment completion. Testing typically occurs every three to four months during the first two to three years after treatment completion and then every six months thereafter. Changes to this schedule may be made during the process of follow-up evaluation.
How will I know if the treatment is working?
Serial PSA blood tests will be used to monitor your progress after definitive treatment of your prostate cancer. Following proton therapy, your PSA will fall but will not reach its lowest value, or nadir, immediately after treatment. Though infrequent, it may take up to two to three years for the PSA to reach its nadir.
This does not mean that PSA testing should be abandoned at this time. It remains an important monitoring tool and serial testing at regular intervals is critical to its effective use. Your doctor will evaluate additional data in conjunction with the PSA to monitor your treatment outcome.
Will I need additional treatment?
Usually, no additional treatment is needed after radiation therapy. The need for additional treatment is determined by the PSA, Gleason score and stage of the prostate cancer and having your daily treatments as scheduled, particularly for external beam radiation therapy (EBRT). Regular post-treatment PSA evaluation plays an important role in monitoring and evaluating the need, if any, for additional treatment in the future.
If cancer recurs, options for treatment will, in part, depend upon the initial treatment. Additional or alternative forms of radiation therapy, prostatectomy, cryotherapy, hormone therapy or any of several treatments under evaluation in clinical trials may be recommended. Your team of doctors, including a radiation oncologist, urologist and medical oncologist, will discuss treatment options and recommendations with you.
Proton therapy for Prostate Cancer
Proton Therapy. A New Era in Cancer Care
Proton therapy is a type of non-invasive radiation therapy that is an incredibly precise cancer treatment that uses a beam of protons moving at very high speeds to destroy the DNA of cancer cells, killing them and preventing them from multiplying. Proton therapy is a revolutionary modality to treat certain patients with prostate cancer. For more than one-half of a century, the idea of using energized protons to treat cancer has been evolving in the laboratories of physicists and medical scientists around the world. Advancements in imaging, along with the development of improved treatment delivery technology and sophisticated computers in recent years, made it possible for Proton Beam Therapy to be available in the established medical centers now. Prostate cancer is the most common indication for proton therapy worldwide.
The Power of Proton Therapy over Conventional Radiation
Conventional radiation therapy uses photons to treat tumours. Photons radiate not only tumour cells but also everything in their path, including healthy cells and structures around and behind the tumour.
Proton therapy uses high energy protons to treat tumors instead of x-rays. In contrast to conventional radiation, Protons can be made to stop in the tumor where they deposit their entire energy enabling complete tumor destruction. Because protons deposit nearly their entire energy in the tumor, there is no radiation beyond the tumor. This characteristic results in no or very minimal damage to surrounding healthy cells making them safer compared to conventional radiation.
How does Proton Therapy work?
Proton therapy uses pencil beam scanning to deliver radiation and match each tumour’s exact shape and size in three dimensions. This allows a single layer of a tumor to be treated at a time, in effect painting the tumor with radiation layer-by-layer and slice-by-slice until the entire area has been treated.
How are protons produced?
Protons are produced in a machine called the cyclotron. They are then released, from a gantry, in a sharp beam (approximately 3 mm in size); the latter may vary depending on various factors. The energy of the proton beam varies with the depth of tissue/ tumour that has to be treated. Each energy form treats a layer of tissue as a series of spots. The position of the gantry is changed to access the tumour from various directions for accurate delivery of the proton beam, without compromising the safety of adjacent normal tissue.
What are the benefits of Proton Therapy?
Because it involves significantly less radiation exposure to normal tissues, proton therapy lowers the risk of side effects and secondary, radiation-induced cancers. Proton therapy, alone or in combination with other treatments, may be a great choice for many specific types of cancers and benign conditions. Additionally, proton therapy can treat recurrent cancers and also children with cancer. It is also an important treatment option for cancers that cannot be completely removed by surgery. This advanced technology:
- Gives better protection to surrounding healthy tissues
- Lowers the risk of radiation-induced secondary cancers
- Results in fewer side effects and better quality of life
Why should you choose Proton Therapy for Prostate Cancer?
Proton therapy is one of the most effective forms of treatment for prostate cancer. Proton therapy may be used as the only treatment or can be combined with hormonal therapy or after other treatments, such as surgery, to manage cancer that has recurred or is at high risk of recurrence.
Proton therapy has an excellent record of success, providing long-term disease control and survival rates equivalent to other treatments, including surgery. Several research studies published in leading scientific journals have reported very low genitor-urinary, gastrointestinal and sexual function related toxicities with proton therapy. Several patients prefer proton therapy due to its non-invasive nature and minimal, or no adverse effect on their quality of life.
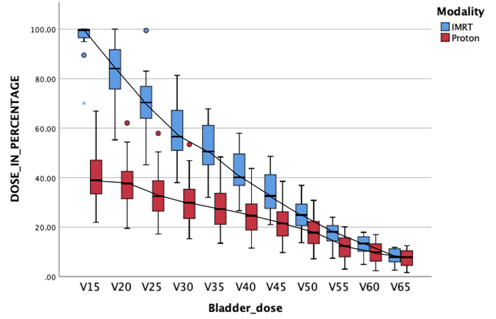
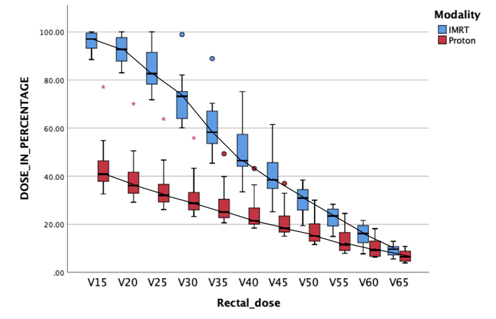
As per our experience at APCC, proton therapy ensures the least possible doses to the urinary bladder and rectum. The below picture represents a dose comparison between proton therapy and IMRT. Better sparing of the dose to healthy normal urinary bladder as well as the rectum is obvious with proton therapy.

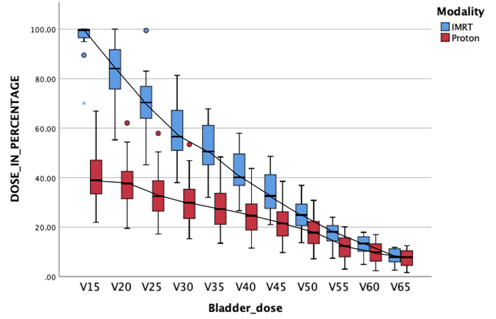
Bladder dose comparison between IMRT and Proton therapy: Lesser the dose to bladder, lesser is the urinary toxicity related to urinary bladder irradiation.
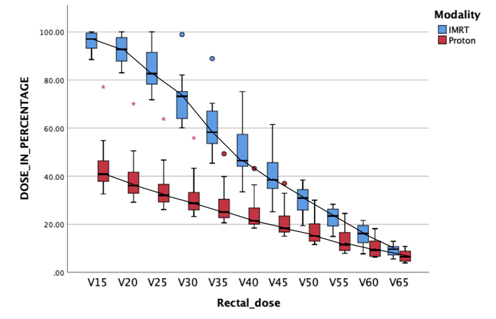
Rectal Dose Comparison between IMRT and Proton therapy: Lesser the dose to the healthy rectum, lesser is the rectal toxicity.
How do you prepare for Proton Therapy?
Before you undergo proton therapy for prostate cancer, your care management team guides you through a planning process to ensure that radiation reaches the precise spot in your body where it's needed. Accurate planning is essential for the use of all radiation therapy, but especially so for Proton therapy. The goal is to precisely deliver radiation to cancer while minimizing damage to surrounding healthy tissue.
What can I expect during proton therapy?
Undergoing proton therapy is similar to having a routine X-ray. Proton therapy cannot be seen, smelled, or felt.
In Proton therapy, the patient is treated on an outpatient basis and the therapy will be administered five days a week over about four to eight weeks. Each treatment session usually lasts less than an hour, most of which is the preparation time. The actual radiation treatment takes only a few minutes.
How should I expect to feel after proton therapy?
After completing proton therapy, urinary and bowel side effects may persist for two to six weeks, but they will improve over time. You may need to continue some medications.
Other minor problems may include dry itchy skin, a sensation of heaviness in the perineum, anal and rectal irritation, and a flare-up of hemorrhoids. However, patients are usually well enough to continue with normal daily activities.
Large series of patients treated with proton therapy published a few years ago showed excellent sexual function in patients in younger than 60 years.