When treating cervical cancers, the aim of modern radiotherapy techniques is to ensure that the uterus, its adjacent pelvic structures and the pelvic lymph node bearing region receive the correct dose. An additional and equally important aim is to ensure that the normal organs in the vicinity i.e., the urinary bladder, rectum, small and large bowel, and bone marrow, receive the least possible dose. This is done to ensure that the toxicity of radiation is kept at the minimum possible.
Irradiation of these of the above mentioned structures leads to short term and long term consequences such as inflammation of the bladder, diarrhoea, narrowing of the gut, bleeding in the urine and stool and risk of insufficiency fractures.
The side effects can be minimised by reducing the doors to all these structures.
At Apollo Proton Cancer Center, the options for delivering safe and accurate radiotherapy are theRadixact Helical Tomotherapy Unit and Proteus Plus proton therapy unit.
The Radixact helical tomotherapy machine is a sophisticated linear accelerator which has inbuilt features that ensure that patient undergoes imaging I,e a CT scan prior to delivery of treatment every day. The radiation is delivered in successive narrow segments as the patient moves through the machine which allows the treating team to spare normal organs very effectively.
Proton therapy has a unique characteristic in that protons, which are positively charged particles, deposit their entire energy at a predefined target and tissues distal to the target receive no radiation. This allows better sparing of the normal organs. In endometrial cancer patients, this results in smaller doses to the small bowel, large bowel, bone marrow and urinary bladder. The expected outcome of this is reduction in the risk of diarrhea, narrowing of the bowel and inflammation of the bladder. In addition, since the pelvic bone marrow is being spared, there is better tolerance of treatment delivered along with or after chemotherapy. This is especially relevant in the elderly. In young patients, there is the additional benefit of reduction in the risk of radiation induced second cancers because of decrease in low dose radiation being received by normal structures.
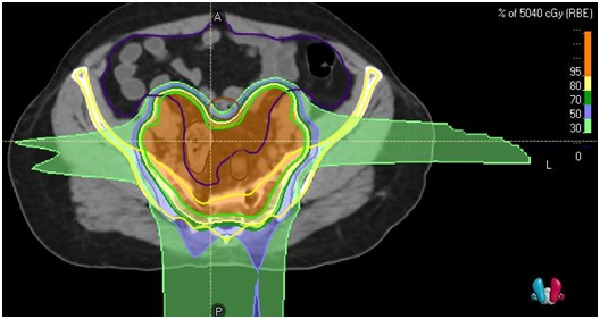
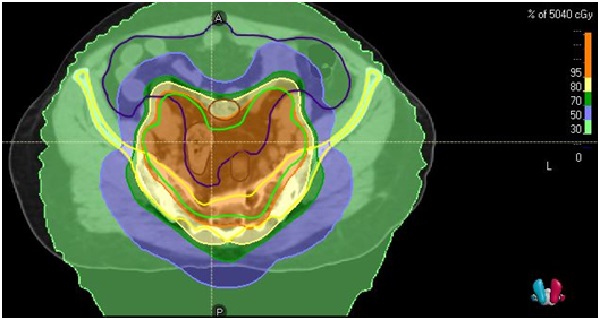
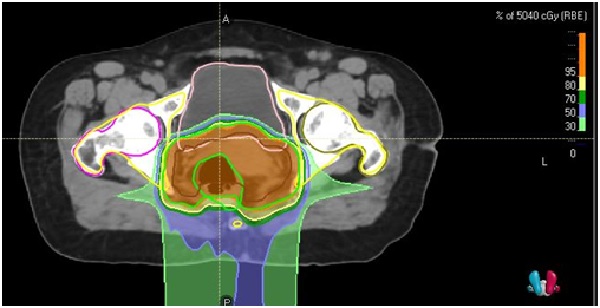
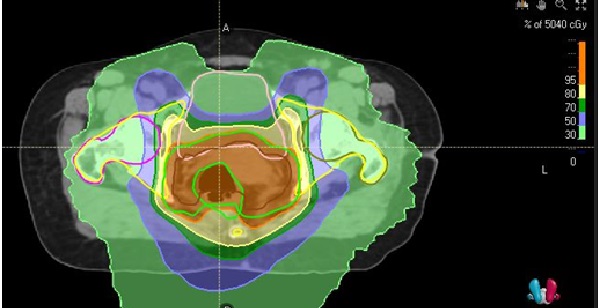
The target for this patient suffering from cancer cervix is outlined in green.
The lavender colourwash represents 50% of the prescribed dose. The green colourwash represents 30% of the prescribed dose.
The 50% and 30 % dose clouds spare the bone marrow (white arrow) and the intestines (red arrow).
In this plan, with proton therapy the average dose received by the bladder is and bone marrow are
approximately 55-60% of the dose received in the Tomotherapy plan.
Similarly, the average dose received by the intestines in proton therapy is half of that received during photon based treatment.
Since the risk of side effects like severe diarrhoea, cramps, cystitis and low blood counts is dose linked, this reduces the probability of these side effects.
All patients receive treatment with diligent attention to ensuring least possible dose to normal organs by following daily bladder filling protocols; a filled urinary bladder displaces bowel for the region being treated, thus protecting it.
At present, Vaginal brachytherapy services are not available at Apollo Proton Cancer Centre.
The treatment of cancer of the vagina is similar to that of cancer cervix.